
Tiny Tricks Battle Brain Cancer
What's in the Story?
The ancient city of Troy was well protected by its high stone walls and strong wooden gates. This city was so well secured that it was actually considered invincible. According to the legend of Troy, Greek soldiers came up with a trick to breach the fortress walls. Hiding themselves in a giant wooden horse that they gave to the city as a gift, the Greek invaders got behind the city walls and conquered Troy.

This legend became so well known that we adopted the term “Trojan horse” as a word for any trick that allows us to secretly breach a protected place. Perhaps a team of scientists that studies brain cancer was inspired by the Greek legend. The scientists have been working on how to smuggle special medicine for brain cancer through the blood-brain barrier. The blood-brain barrier is a strong wall that shields the brain from all kinds of dangerous particles.
In their Nature Materials article “P-selectin-targeted nanocarriers induce active crossing of the blood–brain barrier via caveolin-1-dependent transcytosis” they discuss how they learned to cross this barrier in mice.
Protecting the Brain
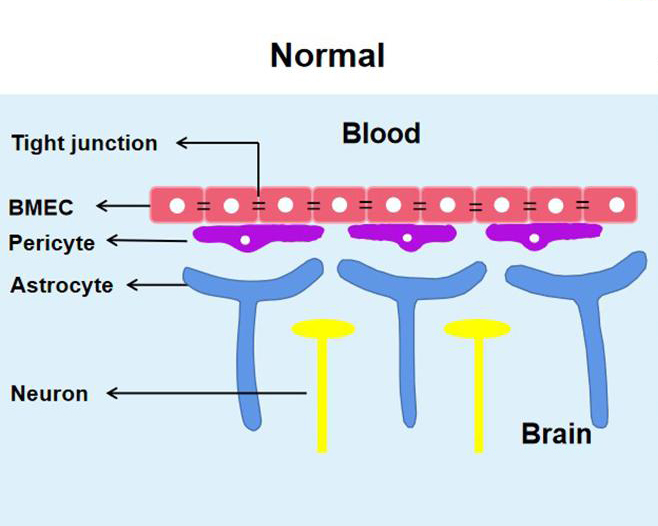
The brain is protected like a fortress behind the walls of what scientists call the blood-brain barrier. This barrier is made of tightly packed tissue that contains many cell types and that surrounds the blood vessels in the brain. It shields the brain from dangerous bacteria or viruses that may be circulating in the blood. But what is meant to protect the brain from danger is also a major obstacle in the treatment of brain tumors.
The blood-brain barrier keeps many cancer drugs out of the brain. A few drugs can cross the barrier but do it so poorly that patients need to take very high doses and often suffer severe side effects. Brain cancer patients would majorly benefit if their cancer drugs could cross the barrier more easily.
Nanoparticles - Cancer Drug Shuttles
To try to improve delivery of cancer drugs to the brain, a group of scientists tested a trick to treat medulloblastoma. This cancer is the most common malignant brain tumor in children. To do this, they packed the drug into a sort of Trojan horse, in this case, nanoparticles, which are tiny bubbles that can carry medicine.
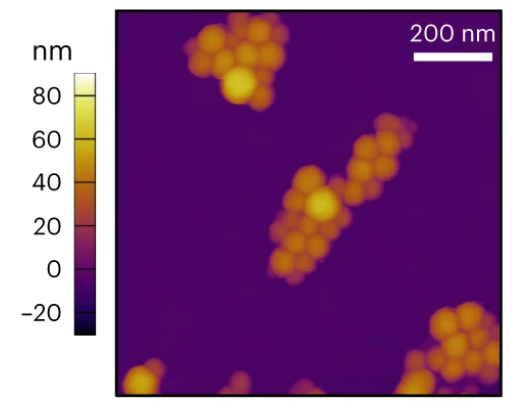
The scientists designed a special surface on the nanoparticles. This allows them to send the particles to the desired destination in the body. You can think of it as writing the address on a package before taking it to the post office. The address in this case would be p-selectin, a molecule that is found in high numbers on the inner surface of tumor blood vessels.
Energy and nutrients are distributed to all organs by blood vessels. Tumors use a lot of nutrients, and so they often have extra blood vessels that supply them with energy. However, tumor blood vessels differ from blood vessels in healthy organs. One difference is that tumor blood vessels have a lot of p-selectin on their inner surface. This molecule is usually associated with injury and helps attract immune cells. They also make more p-selectin in response to tumors. The tumor blood vessels make even more p-selectin when treated with special rays called radiotherapy. These rays are a type of cancer treatment and are used to kill cancer cells. Almost every brain cancer patient receives this treatment.
Thanks to their special surface, the nanoparticles find their molecular address (p-selectin) in the tumor blood vessels. They then gather in the tumor blood vessels outside of the blood-brain barrier.
Traveling Nanoparticles
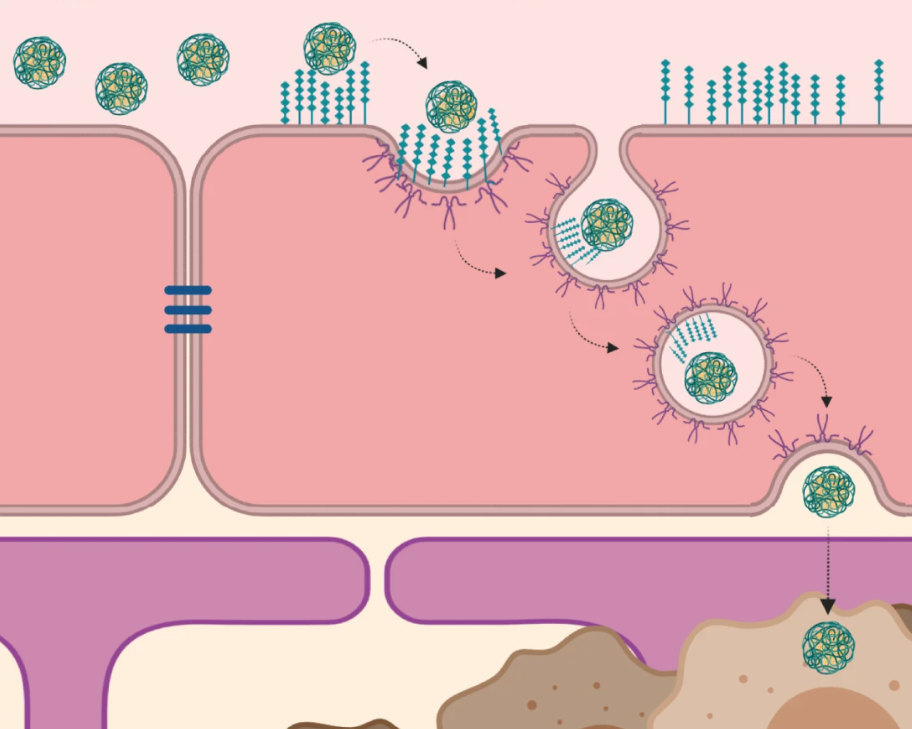
After the nanoparticles arrive in the tumor blood vessel, they have to cross the blood-brain barrier to get into the tumor tissue. Imagine you encounter a big wall that is in your way, and suddenly you discover a secrete passage through the wall. The scientists found that this happens to the nanoparticles. The nanoparticles that bind to p-selectin in the tumor blood vessels are granted access through the barrier.
This movement is called transcytosis. The blood vessel cell “swallows” the nanoparticle that it wants to move. Then, the nanoparticle travels through the cell, until it comes out on the other side, like a secret passage. On the other side it can reach the tumor, where it releases its cargo.
Drug-filled Nanoparticles
The scientists wanted to compare if their Trojan horse works better than the treatment with the bare drug. They treated mice that had brain tumors with special beams, or so-called radiotherapy. Radiotherapy is part of the standard therapy that is given to most brain cancer patients.
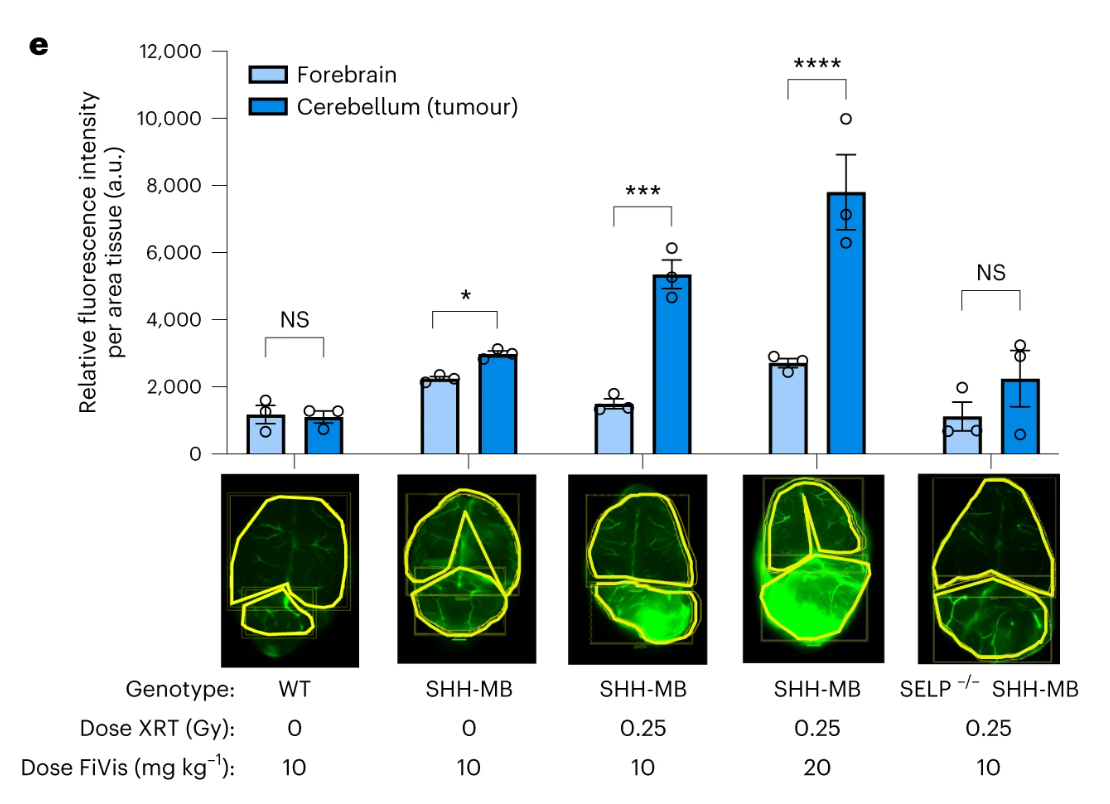
On top of radiotherapy, some mice got the cancer drug packed into nanoparticles. This double treatment made those mice live almost twice as long than the mice that only got the rays by themselves. Other mice got radiotherapy and the same amount of medicine without using the tiny particles to pack it up. In this case, the medicine didn't slow down the tumor growth at all. It was as if these mice had only gotten radiotherapy.
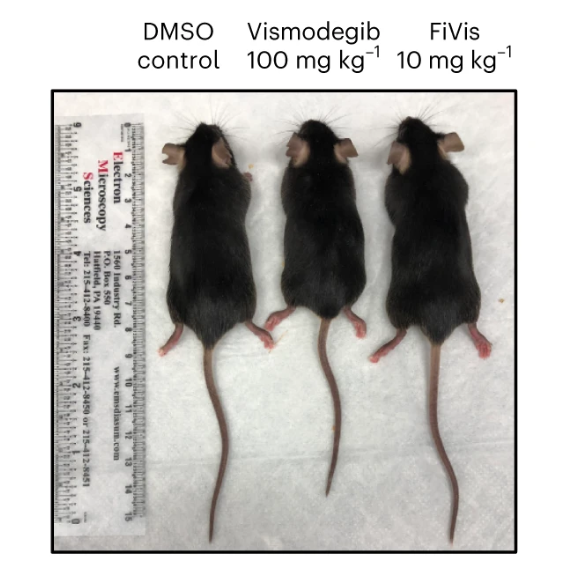
The scientists explain that they would have to give the “free” drug (not packaged in a carrier) in at least five times higher doses to see a healing effect. However, higher doses of the free drug result in side effects that aren’t good for the patients. One side effect of high doses in mice is that their bones do not grow normally, and they can end up with shorter legs.
When the scientist treated the mice with drug-filled nanoparticles, they did not observe any bad side effects. They hope that in the future, brain tumor patients can be treated with medicine that is packed into nanoparticles. The team of researchers is convinced that this will help improve brain cancer therapy and reduce side effects. More testing is needed to make sure that the nanoparticles are safe for human patients.
So it turns out that using tiny particles to carry medicine to brain tumors could be really helpful. And the benefits of targeting p-selectin goes beyond brain tumors. Nanoparticles may be able to find other tumors as well and may help to treat cancers at other sites around the body.
Additional images via Wikimedia Commons. Menu MRI image by Bobjgalindo.
Bibliographic details:
- Article: Tiny Tricks Battle Brain Cancer
- Author(s): Tanja Eisemann
- Publisher: Arizona State University School of Life Sciences Ask A Biologist
- Site name: ASU - Ask A Biologist
- Date published: 14 Dec, 2023
- Date accessed:
- Link: https://askabiologist.asu.edu/plosable/nanotools-for-cancer
APA Style
Tanja Eisemann. (Thu, 12/14/2023 - 14:53). Tiny Tricks Battle Brain Cancer. ASU - Ask A Biologist. Retrieved from https://askabiologist.asu.edu/plosable/nanotools-for-cancer
Chicago Manual of Style
Tanja Eisemann. "Tiny Tricks Battle Brain Cancer". ASU - Ask A Biologist. 14 Dec 2023. https://askabiologist.asu.edu/plosable/nanotools-for-cancer
Tanja Eisemann. "Tiny Tricks Battle Brain Cancer". ASU - Ask A Biologist. 14 Dec 2023. ASU - Ask A Biologist, Web. https://askabiologist.asu.edu/plosable/nanotools-for-cancer
MLA 2017 Style

The blood-brain barrier is a special layer of cells that surrounds the blood vessels of the brain. While it protects us from many toxins, it can also make treating cancer in the brain more difficult. What are scientists doing to try to get around this important shield?
Be Part of
Ask A Biologist
By volunteering, or simply sending us feedback on the site. Scientists, teachers, writers, illustrators, and translators are all important to the program. If you are interested in helping with the website we have a Volunteers page to get the process started.
